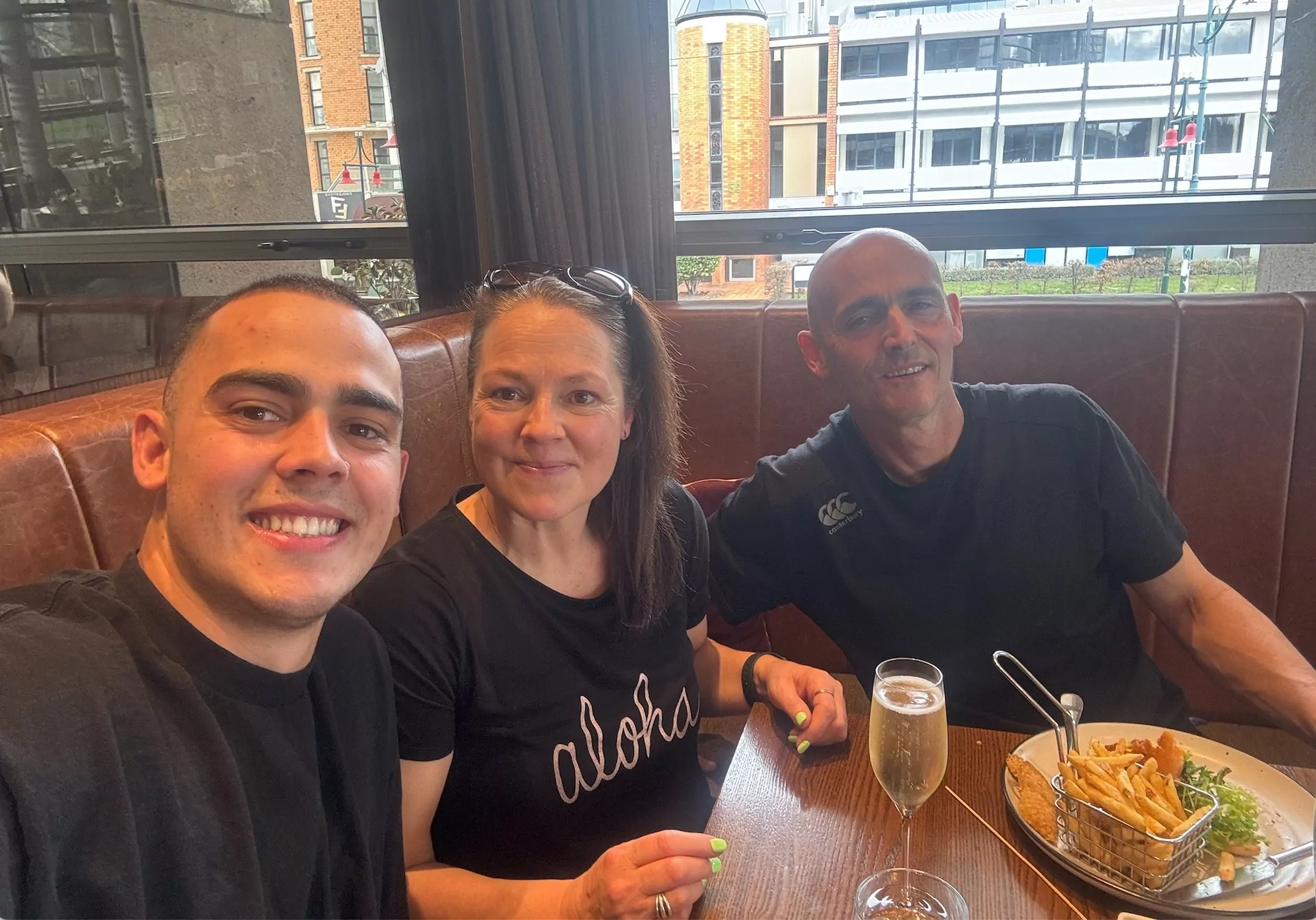
Photo: Supplied
A Christchurch woman with a potentially fatal skin condition says the public health system failed her.
Karen’s face became badly infected after her young grandson accidentally cut her with glass in March just below her eye.
She sought medical help at local clinics, but after weeks, her face become worse.
“I was given lots of different antibiotics, but nothing worked.”
Karen’s condition got so bad she was forced to go to the emergency department.
“Basically I had all this stuff all over my face and it was just kind of a sticky ooze. The staff at ED were lovely and referred me to the eye clinic.
The doctor there took one look at me and said what the hell have you got on your face?
He thought it was cancer, so the first thing he did was take a biopsy.”
Karen said the results were negative, but that provided no peace of mind because her face wouldn’t heal.
“I was really concerned that there was still stuff coming out of my eye. There was another hole in my eye”
Karen returned to ED and was again referred back to the eye clinic, which then referred her to the Dermatology Department at Christchurch Public Hospital.
“I saw a dermatologist a few times, but she left and I had no one. They managed to find me a retired consultant, who was working from home but could only see me over FaceTime.
She managed to book me for an infusion at the hospital, to kill my T cells and followed up by organising special creams for my face.
“After my second infusion, I was suddenly told the dermatologist was no longer working there anymore, and they decided to close the department.
“I thought to myself I’m going to die?”
The receptionist on the phone said the public doesn’t know what’s going on, we don’t even know what’s happening, and we’re sitting here with nothing to do. We have no consultants.”
Karen said she became depressed at the thought of an uncertain future with a huge infection on her face.
“I thought to myself I’m going to die? I’ve got no one to help me. I was so angry about the fact that they thought it’s perfectly acceptable to close one department.”
Karen sent a letter to Health Minister Andrew Little, but never heard back.
Chris Lynch Media approached the minister’s office for comment but was referred to Te Whatu Ora Waitaha.
Out of desperation, Karen turned up, unannounced at Ken MacDonald Surgery on Bealey Avenue, and pleaded with staff to be seen. Dr. MacDonald managed to see Karen straight away.
Dr MacDonald told Chris Lynch “this patient had neglected and advanced pemphigus, a complex dermatological condition which has a 99% mortality rate if it is not treated in a timely and effective way.
Pemphigus causes a terrible death with the loss of skin (like a full body burn) and detachment of the membranes covering the eyes and mouth.”
Karen said she was extremely lucky. “I take my hands off to those people because they turned my life around. They went above and beyond and were absolutely fantastic.”
Dr MacDonald said “there is no dermatology service now in Christchurch and no pathway for referrals to other parts of the country.
This is entirely the fault of hospital management who never took things seriously and never created a proper department despite knowing that they had to.
Excuses like they tried to appoint dermatologists or dermatologists just resigned don’t wash.”
Dr Ken MacDonald said there was a “total management failure” at Te Whatu Ora Waitaha (Formerly the CDHB) Photo: Chris Lynch
Dr MacDonald said “the responsibility for this lies with the management of the recently disbanded CDHB, many of whom are still in position and need to answer to this.
An example of the total management failure was the loss of a young and very respected specialist dermatologist who did not have an operating theatre light and was told he could get a headlamp from Kathmandu and request a refund of costs.
This doctor had a surgical fellowship and MD thesis in the treatment of complex skin cancer and had spent years acquiring New Zealand equivalent qualifications – but he was simply not given the time of day by management and resigned.
To cut to the chase, dermatology does not need any managers – they should all be replaced by doctors and nurses.
A dermatology department, essentially covering the entire South Island, would need four or five other dermatologists to support the head of the department as well as other junior staff.
Te Whatu Ora Waitaha Canterbury Chief Medical Officer Dr Richard French confirmed there was no specialist medical Staff due to recent resignations.
“We are referring patients to General Practice care, and our Plastic Surgery and Rheumatology teams are supporting where their scope of practice allows.”
Dr French said “we have been recruiting actively both nationally and internationally for several years now but unfortunately, there is a severe shortage of dermatologists in New Zealand and worldwide.”
Regular discussions were being led by the Ministry of Health on strategies to address the workforce issue going forward.
He said the hospital was working to secure registration and a visa for a new overseas trained Senior Medical Officer to join the Dermatology Service.
He is expected to arrive in New Zealand in January and will spend six weeks in Auckland to meet the supervision requirements of the Medical Council.
“We have previously reached out to private dermatology services to see if they can offer support, but unfortunately the private sector is reporting that it is at capacity and cannot assist the public service. There are ongoing discussions about a national model of care to build a sustainable public dermatology service across New Zealand.”
Dr French said the hospital have some trainees who are part way through their dermatology training in Auckland, and who will return to work in Christchurch on completion of their training.